The Medicaid Redetermination process is likely to result in many eligible beneficiaries losing their coverage. This blog explores how conversational AI and automation can improve the redetermination process. By examining the benefits of conversational AI, such as its ability to provide personalized assistance, reduce administrative burden and increase accuracy and efficiency, this blog aims to demonstrate how this technology can result in better redetermination outcomes.
The State of Medicaid After the Pandemic
Medicaid is the largest health insurance program in the United States, covering more than 70 million people before pandemic. At the beginning of the COVID-19 pandemic, Congress enacted the Families First Coronavirus Response Act (FFCRA), which required Medicaid programs to keep people enrolled in the program continuously until the end of the public health emergency (PHE). Due to the continuous enrollment provision, Medicaid enrollment has grown substantially compared to before the pandemic with more than 92 million enrollees, an increase of more than 22 million from February 2020 to December 2022.
For the duration of the continuous enrollment provision, states had paused most Medicaid terminations and eligibility reviews. This means that states need to renew coverage for more than 92 million enrollees within the next 12 months. Without assistance from technology, such as conversational AI, the burden of renewal will fall upon already-strapped administrative staff.
What is Medicaid Redetermination?
 Medicaid redetermination is the process by which states ensure that Medicaid enrollees continue to meet the eligibility requirements for coverage. Medicaid is jointly funded by state and federal governments. This means that Medicaid eligibility varies from state to state.
Medicaid redetermination is the process by which states ensure that Medicaid enrollees continue to meet the eligibility requirements for coverage. Medicaid is jointly funded by state and federal governments. This means that Medicaid eligibility varies from state to state.
Generally, to be eligible for Medicaid, a person’s income must meet minimum threshold, and some populations are also subject to asset tests. States are required to periodically redetermine enrollees’ eligibility and disenroll those who no longer meet the eligibility requirements.
Impact for Various Stakeholders
HHS projects that about 15 million Medicaid enrollees will lose their coverage during the redetermination process. Disenrollment will not happen at once but rather spread out through 2023 and early part of 2024. HHS further projects that approximately 7 million enrollees will lose coverage due to procedural reasons (i.e., not because they are actually ineligible). A lapse in coverage could make it difficult for enrollees to access care that they need and could also lead to worse health outcomes.
For some states, this means that they need to mail a renewal form or document request to enrollees that cannot be renewed administratively (verifying eligibility through available data sources such as state wage databases). Furthermore, they cannot simply disenroll someone if mail is returned as undeliverable; they must make a good faith attempt to find the person. With an average vacancy rate for Medicaid agencies at 17% in FY2022, this puts immense pressure on available staff.
Managed Care Organizations that administer Medicaid and CHIP plans stand to lose revenue that they would get from covering these enrollees. Additionally, they will need to spend time and resources to process disenrollment and appeals against disenrollment.
Providers also stand to lose thousands of Medicaid patients if patients do not verify their eligibility requirements to State Medicaid agencies.
Reduce Coverage Gaps with Conversational AI
Medicaid agencies cannot tackle redetermination alone. New Medicaid enrollees that came into the program during the continuous enrollment provision may have never experienced redetermination and may not know that their coverage is at risk. The task of communicating with beneficiaries can be amplified by a variety of stakeholders, including Managed Care Organizations, providers, advocacy organizations and others that have frequent communication with Medicaid enrollees. This will reduce the number of enrollees who are disenrolled due to a failure to respond to agency requests for updated enrollee information.
Proactively Educate Enrollees with Conversational AI
Medicaid agencies, MCOs and Healthcare providers can all proactively reach out to Medicaid enrollees with communications on educating the enrollees about the redetermination process and getting them to update their information on agency portals. Particularly, MCOs and providers may have more updated contact information for enrollees. In addition to sharing this information with Medicaid agencies, they can use Intelligent Virtual Assistants (IVAs) to contact enrollees with a personalized outreach and educate them about the process and the steps that they need to take to ensure that their contact information with Medicaid agencies is updated. With IVAs, they’re able to automate outreach without additional overhead costs.
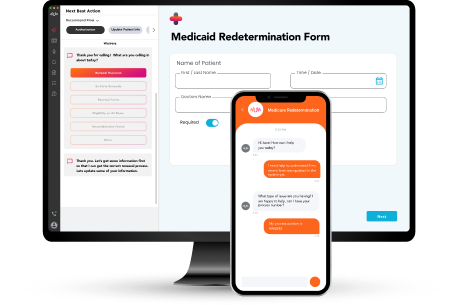 Similarly, for incoming calls, MCOs and providers can deploy IVAs. These IVAs identify the callers who are enrolled in Medicaid and educate them about the redetermination process. The effectiveness of IVAs can be significantly enhanced with multimodal capabilities that visually guide enrollees on their smart devices to agency portals and provide guidance on other steps that are needed to maintain coverage.
Similarly, for incoming calls, MCOs and providers can deploy IVAs. These IVAs identify the callers who are enrolled in Medicaid and educate them about the redetermination process. The effectiveness of IVAs can be significantly enhanced with multimodal capabilities that visually guide enrollees on their smart devices to agency portals and provide guidance on other steps that are needed to maintain coverage.
Assist Agents in Real Time to Support Enrollees with Redetermination
Medicaid agencies are already facing staff shortages and are expected to bring in new workers to help with the redetermination case load. As enrollees call in response to the redetermination notices, real-time agent assistance can help case workers with the resources that they need to make accurate and timely decisions. With real-time agent assistance, case workers can review enrollee information and identify potential problems, such as missing information or inconsistencies, and guide callers on gathering the necessary information.
For MCOs and providers, real-time agent assistance can identify the callers who are Medicaid enrollees and provide agents with real-time guidance for a conversation on the redetermination process. Through real-time guidance, agents can evaluate callers’ awareness of process, and provide personalized guidance on how to navigate the redetermination process. For beneficiaries that are no longer Medicaid-eligible, real-time assistance guides agents to help members find alternative coverage options.
Engage in Root Cause Analysis Using Actionable Insights
During redetermination, performance monitoring is vital to understanding if the process is clear to enrollees and where there are bottlenecks leading to procedural disqualifications. Contact centers are going to be an important touchpoint for beneficiaries – many of whom will be experiencing this process for the first time. By analyzing 100% of every call center conversation with conversational AI, agencies will understand the effectiveness of communications, challenges faced by enrollees and call reason trends. This can make a material difference to health outcomes for the roughly 7 million enrollees who are likely to lose coverage due to procedural reasons.
A lapse in coverage for eligible beneficiaries will lead to health issues that will be expensive and painful to fix—for agencies, MCOs, providers and beneficiaries down the line. Advanced conversational AI and automation can help agencies and MCOs in assessing the redetermination process, avoiding costly mistakes and improving health outcomes efficiently and at scale.
)
